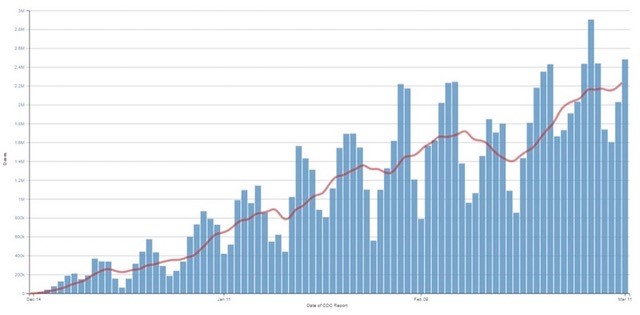
As of Sunday evening, March 14, the CDC reported that almost 70 million people, some 21% of the US population, have received at least one dose of a COVID-19 vaccine. More than 37 million Americans, or 11.3% of the population, have been fully vaccinated. The CDC’s Data Tracker breaks down those vaccinations by demographic here: https://covid.cdc.gov/covid-data-tracker/#vaccination-demographic.
As of March 11, the seven-day average for new shots in arms reached 2.2 million, an 8% increase over the previous week. See https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html.
(See this Bloomberg tracker for latest numbers: https://www.bloomberg.com/graphics/covid-vaccine-tracker-global-distribution/?sref=TG2o5EVv.)
The vaccine race is picking up speed, and that’s good news. Vaccination rates, of course, vary by state, with New Mexico in the lead with 26.1% vaccinated as of March 10 and Georgia trailing dead last as of that date, with 13.4% vaccinated (https://fortune.com/2021/03/10/covid-vaccine-pfizer-moderna-johnson-johnson-numbers-by-state-coronavirus-vaccines-shots-doses-given-us-latest-update/).
The very good news about vaccines, including the addition of the Johnson & Johnson vaccine, is, however, counterbalanced by the presence and the spread of COVID variants of concern in the US. The CDC maps where these variants are being found, but since not every COVID case is genetically sequenced (that testing needs to expand dramatically), the numbers are merely indicators as to where variants have gained a foothold. The map below is interactive at the CDC site and tracks B.1.1.7 (shown here), P.1, and B.1.351. (https://www.cdc.gov/coronavirus/2019-ncov/transmission/variant-cases.html)
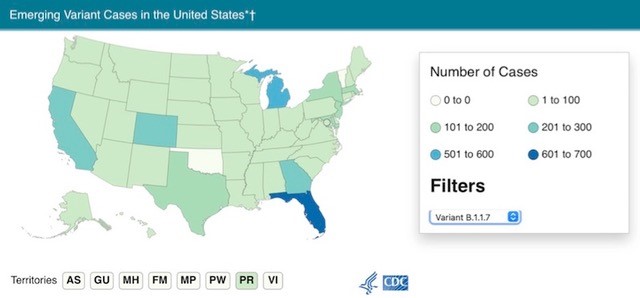
Despite medical objections and the challenges variants pose, states such as Texas and Mississippi have joined others, such as Florida, in questionable policies and public behavior; and so masking and mitigation stand to be defeated by spring break behavior. In a few weeks we’ll know whether disease and deaths spike or not. Wide open for spring break, Florida will be a test case as the more contagious and 30% more deadly variant B.1.1.7 circulates in a cauldron of residents and visitors, masked and unmasked, as vaccinations continue. The B.1.1.7 variant is on track to become the dominant strain in Florida, as it has in Europe, sometime this month (“UK coronavirus variant on track to become dominant strain in Florida,” https://www.fox13news.com/news/uk-coronavirus-variant-on-track-to-become-dominant-in-florida).
Writing for STAT, Andrew Joseph and Helen Branswell (who won a Polk Award last month for her reporting on the pandemic) offered earlier this month a balanced, well-informed look at the path ahead: “However long it takes, the transition to a mild endemic virus is unlikely to be a straight line. Some infectious disease researchers envision a healthier summer – with low circulation of the virus and more people vaccinated – but a more tenuous fall. Other factors, like how long protection provided by vaccines will last, what percentage of people gets them, and whether variants of the virus sap the strength of vaccines, will determine the outcome.” Their analysis, “The short-term, middle-term, and long-term future of the coronavirus,” is well worth a read. See https://www.statnews.com/2021/03/04/the-short-term-middle-term-and-long-term-future-of-the-coronavirus/.
One aspect of the COVID pandemic that has enormous implications, beyond vaccine and variants, is its capacity to significantly undermine the health and well-being of those who tangle with it, not just for weeks but for many months. On Monday, March 15, Wall Street Journal reporter Sumathi Reddy profiled several COVID “long haulers” who have been sick for a year and the concerted efforts being made to help long haulers get better. According to Dr. David Putrino, director of rehabilitation innovation at Mount Sinai, most long haulers will need four to six months of rehabilitation. Improvement is, at best, uneven and gradual. (“They Got Covid One Year Ago. They’re Still Sick,” https://www.wsj.com/articles/they-got-covid-one-year-ago-theyre-still-sick-11615838402)
About 10% of those who are infected with SARS-CoV-2 find themselves profoundly impacted by “long COVID,” suffering lasting symptoms that impair their ability to function as they once did (“As Their Numbers Grow, COVID-19 “Long Haulers” Stump Experts,” https://jamanetwork.com/journals/jama/fullarticle/2771111), while around 30% appear to have at least some symptoms that last six months or more and that impact their quality of life (“Sequelae in Adults at 6 Months After COVID-19 Infection,” https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2776560).
For many, then, a bout with COVID doesn’t end when active infection does. Some long haulers manage to keep working; for others holding a job or even managing daily tasks at home becomes entirely too much. Meanwhile, their medical costs continue to mount. As US confirmed COVID cases near 30 million, the math says we may have some 3 million “long haulers” in the US alone. Dozens of clinics have already been established across the US, from New York to L.A., to treat them (“‘We know this is real’: New clinics aid virus ‘long-haulers,’” https://www.modernhealthcare.com/providers/we-know-this-real-new-clinics-aid-virus-long-haulers).
Long COVID finally has an official name – Post-Acute Sequelae of SARS-CoV-2 (PASC) – and will be the subject of an intensive study. Neurological symptoms are a particular focus for the NeuroCOVID project, a databank that will aggregate data on COVID patients of all ages. (“Dr. Anthony Fauci aims to answer 'a lot of important questions' about 'COVID long-haulers' in new nationwide initiative,” https://www.usatoday.com/story/news/health/2021/02/24/covid-19-long-haulers-fauci-announces-launch-nationwide-initiative/4572768001/)
In the compilation that follows, we invite readers to take a closer look at “long haul” COVID and its impacts, both economic and personal. Once you review it, you may see why we continue to favor a multifaceted overweight healthcare position. At Cumberland we remain overweight the healthcare sector, including pharmaceutical, biotech, and medical devices. Unlike the partying hordes on Siesta Key, we think COVID is not over. And even when it is, for millions it will continue to cast a long shadow into the future.
The Economic Burden
Just as there are many medical questions yet to answer about long COVID, or PASC, there are also many questions to answer about the costs that COVID’s longer-term health impacts will impose. Those obviously include medical bills, insurance costs, disability costs, careers temporarily or permanently derailed and lifelong earnings slashed as a result, as well as lost economic productivity across a population. We don’t have solid numbers yet, but we know they will be big.
There are experts beginning to suggest the scale of costs, at least on the healthcare front. Here are three takes: “Bruce Lee of the City University of New York (CUNY) Public School of Health estimated that if 20% of the U.S. population contracts the virus, the one-year post-hospitalization costs would be at least $50 billion, before factoring in longer-term care for lingering health problems.” (“COVID-19 long-term toll signals billions in healthcare costs ahead,” https://www.reuters.com/article/us-health-coronavirus-fallout-insight/covid-19-long-term-toll-signals-billions-in-healthcare-costs-ahead-idUSKBN24Z1CM)
“‘The economic impact will be much greater if younger survivors endure decades of coronavirus-related disability,’ says Olga Jonas, a former economic adviser at the World Bank who studies the impact of contagions at Harvard. Polio would have led to an estimated $215 billion in treatment costs in the U.S. from 1955 to 2015 had vaccines not become widely available, a 2006 study found.” (“Covid Long Haulers Describe the Devastating Aftereffects of the Disease,” https://www.bloomberg.com/news/features/2020-11-09/coronavirus-long-haulers-tell-us-their-symptoms-and-the-aftereffects-of-disease)
“What’s still emerging is the extent to which the enduring disability will weigh on health systems and the labor force. That burden may continue the pandemic’s economic legacy for generations, adding to its unprecedented global cost – predicted by Australian National University scholars to reach as much $35.3 trillion through 2025 as countries try to stop the virus’s spread.” (“Debilitating Covid-19 Effects and Economic Costs May Linger for Years,” https://www.bloomberg.com/news/articles/2020-08-24/covid-s-lingering-malaise-adds-to-35-trillion-economic-cost)
What We Know about Long Haul COVID (PASC)
News about “long COVID” and “COVID long haulers” has been rolling in for months, and we’ve kept it on our radar. This article offers a relatively up-to-date, succinct overview of what we know about it, from the spectrum of symptoms people suffer to who is more likely to end up a “long hauler” (more women than men, but the young as well as the old: “COVID ‘long-haulers:’ What is PASC, and why do some people get it?” https://www.kiro7.com/news/trending/covid-long-haulers-what-is-pasc-why-do-some-people-get-it/VPPMEKN2BVFXFCCKGMCW2FG77M/.
Dr. Gregory Poland of the Mayo Clinic, who was interviewed for the article, suggests that many are too casual about the risks COVID poses: “People who are thinking, especially young people, ‘(It’s a) mild disease, you know. I might not even have any symptoms, and I’m over it.’ Whoa. The data is suggesting otherwise,” Poland said. “There’s evidence of myocardial damage, cardiomyopathy, arrhythmias, decreased ejection fractions, pulmonary scarring and strokes,” he added.
Interestingly, symptoms seem to appear in waves, beginning with the illness itself. “Long-haul Covid patients can experience 'waves of symptoms,' early research suggests,” https://www.nbcnews.com/health/health-news/long-haul-covid-patients-can-experience-waves-symptoms-early-research-n1259281
Remarkably, even asymptomatic cases of COVID-19 can trigger symptoms that unwind over months. “Many ‘Long Covid’ Patients Had No Symptoms from Their Initial Infection,” https://www.nytimes.com/2021/03/08/health/long-covid-asymptomatic.html
One serious complication of PASC is heart damage, which affects 50% of those hospitalized with the illness (“Heart damage found in half of COVID-19 patients discharged after hospitalization,” https://www.imperial.ac.uk/news/216033/heart-damage-found-half-covid-19-patients/). Even among those who are not seriously ill, damage is not unlikely. A study of two dozen Ohio State football players found that 15% of them had evidence of potentially deady myocarditis, while a further 30 percent had cellular damage or swelling (“College Athletes Experienced Heart Damage After COVID-19: Study,” https://www.the-scientist.com/news-opinion/college-athletes-experienced-heart-damage-after-covid-19-study-67929).
Neurological symptoms are common, including a brain fog that persists and makes cognitive tasks difficult and memory elusive (“COVID's cognitive costs? Some patients' brains may age 10 years,” https://www.reuters.com/article/idUSL8N2HI38G). Brain fog is hardly the only lasting neurological symptom: “Ross Zafonte, chief medical officer at Spaulding [Rehabilitation Hospital in Charlestown, Massachusetts] said he is seeing some patients’ cognitive and brain-related issues last for much longer than expected. That includes depression, memory disorders, and PTSD, as well as muscle and peripheral nerve damage that makes mobility difficult. For some patients, their mental awareness has been slow to recover.” (“Long after the fire of a Covid-19 infection, mental and neurological effects can still smolder,” https://www.statnews.com/2020/08/12/after-covid19-mental-neurological-effects-smolder/)
Children Are Long Haulers, Too
As of Monday, March 15, 2617 cases of COVID-related multi-system inflammatory syndrome in children (MIS-C) have been reported by health departments across the US (“Health Department-Reported Cases of Multisystem Inflammatory Syndrome in Children (MIS-C) in the United States,” https://www.cdc.gov/mis-c/cases/index.html).
Close to 12% of these children, data suggests, go on to incur acute kidney injury (“Acute Kidney Injury Found in Children with COVID-19 and MIS-C,” https://www.businesswire.com/news/home/20210308005578/en/).
Twelve-year-old Maggie Flannery, 19-year-old Chris Wilhelm, and 14-year-old Ava McKinney-Taylor are three youthful long haulers profiled by The New York Times. Ava summed up her situation months into her struggle, which began in back in March 2020: “It’s a little hard to have hope right now,” she said. “We don’t know if this will be a lifelong thing, if this will last a year, or two years or five years. So the future is not looking too bright for me personally.” (“At 12, She’s a Covid ‘Long Hauler’,” https://www.nytimes.com/2020/10/22/well/family/coronavirus-symptoms-kids-children-long-hauler.html)
A Measure of Good News for Long Haulers
A new test for COVID using T-cells, the T-Detect COVID-19 test, can help to identify COVID long haulers who may not have had a positive PCR test to confirm a diagnosis. According to the FDA, “The T-Detect COVID test will be a useful tool to help determine if a person previously had COVID-19. This is especially important for people who may have exhibited symptoms previously or believe they have been exposed but have not tested positive.” (“FDA approves new COVID-19 test that could help ‘long haulers,’” https://www.foxnews.com/health/fda-approves-new-covid-test-that-could-help-long-haulers)
Some long haulers report finding noticeable relief from neurological symptoms after getting vaccinated for COVID. No studies have yet been done to verify whether the vaccine actually helps. (“For Some COVID Long-Haulers, Symptom Relief After a Vaccine,” https://www.usnews.com/news/health-news/articles/2021-03-09/can-a-covid-vaccine-help-long-haul-sufferers)
Others, like Amanda Thebe, fitness expert and menopause educator in Houston, have incrementally found their way back to health, past the profound fatigue that long COVID can produce. Searching for solutions, she found the support group Survivor Corps (https://www.survivorcorps.com) and an online guide to managing post-viral fatigue at https://www.nbt.nhs.uk/our-services/a-z-services/bristol-chronic-fatigue-syndromeme-service/post-viral-fatigue-a-guide-management. Rather than pushing herself and suffering setbacks as a result, Thebe began to take a different approach:
“The post-viral fatigue guide ‘spoke about fatigue, and it talked about working within an energy envelope,’ she says. In other words, doing a little bit less than what you think you can (or should) do is the most helpful strategy. When Thebe wanted to take a walk, she would go out for only five minutes, even if she felt she could last for ten.
“Thebe’s practice became what she calls ‘fitness snacking,’ tiny bits of exercise that made her feel better, but that didn’t push her energy levels at all. Working within that energy envelope was another pivotal moment for Thebe. Along with a commitment to eating the most nutrient-dense food she could and staying hydrated, this approach helped her both physically and mentally. Even better, sharing her approach has helped other COVID long-haulers following Thebe’s social media. ‘It makes them feel like they’re getting small wins as well,’ she says. ‘Over time, those small wins can make a huge difference.’”
Thebe’s story appeared in “COVID Long-Haulers Share Their Roads to Recovery,” https://www.endocrineweb.com/news/diabetes/covid-long-haulers.
Clinicians who have dedicated themselves to the quest of understanding causes of PASC and finding treatments that work are finding some success that can ultimately scale to address urgent medical needs of millions of people whose lives have been compromised or derailed because they have contended with COVID-19 (“Unlocking the Mysteries of Long COVID,” https://www.theatlantic.com/magazine/archive/2021/04/unlocking-the-mysteries-of-long-covid/618076/).
The trajectories of recoveries from PASC vary widely, in part according to the nature of the damage done by the virus in each case. But the more we come to understand about the mechanisms that produce the symptoms and the treatments that help, the greater hope medicine can offer. Where COVID’s long haulers are concerned, the interlude between a COVID infection and substantial recovery, whether that interlude lasts months or years (assuming damage isn’t permanent), will mean medical and disability costs, lost productivity and income, and will require expanded medical research, treatments, and rehabilitation services. The economic price tag for long COVID promises to be high.
David R. Kotok
Chairman of the Board & Chief Investment Officer
Email | Bio
Links to other websites or electronic media controlled or offered by Third-Parties (non-affiliates of Cumberland Advisors) are provided only as a reference and courtesy to our users. Cumberland Advisors has no control over such websites, does not recommend or endorse any opinions, ideas, products, information, or content of such sites, and makes no warranties as to the accuracy, completeness, reliability or suitability of their content. Cumberland Advisors hereby disclaims liability for any information, materials, products or services posted or offered at any of the Third-Party websites. The Third-Party may have a privacy and/or security policy different from that of Cumberland Advisors. Therefore, please refer to the specific privacy and security policies of the Third-Party when accessing their websites. Sign up for our FREE Cumberland Market Commentaries Cumberland Advisors Market Commentaries offer insights and analysis on upcoming, important economic issues that potentially impact global financial markets. Our team shares their thinking on global economic developments, market news and other factors that often influence investment opportunities and strategies.